Overview Of Colonoscopy
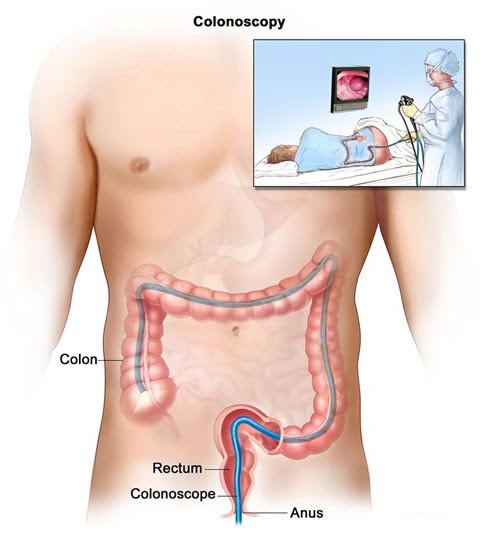
A colonoscopy (koe-lun-OS-kuh-pee) is an exam used to detect changes or abnormalities in the large intestine (colon) and rectum.
During a colonoscopy, a long, flexible tube (colonoscope) is inserted into the rectum. A tiny video camera at the tip of the tube allows the doctor to view the inside of the entire colon.
If necessary, polyps or other types of abnormal tissue can be removed through the scope during a colonoscopy. Tissue samples (biopsies) can be taken during a colonoscopy as well.
What Happens During a Colonoscopy?
The colonoscopy is performed by a doctor experienced in the procedure and lasts approximately 30-60 minutes. Medications will be given into your vein to make you feel relaxed and drowsy. You will be asked to lie on your left side on the examining table. During a colonoscopy, the doctor uses a colonoscope, a long, flexible, tubular instrument about 1/2-inch in diameter that transmits an image of the lining of the colon so the doctor can examine it for any abnormalities. The colonoscope is inserted through the rectum and advanced to the other end of the large intestine.
colonoscopy
Colonoscopy Animation
The scope bends, so the doctor can move it around the curves of your colon. You may be asked to change position occasionally to help the doctor move the scope. The scope also blows air into your colon, which expands the colon and helps the doctor see more clearly.
You may feel mild cramping during the procedure. You can reduce the cramping by taking several slow, deep breaths during the procedure. When the doctor has finished, the colonoscope is slowly withdrawn while the lining of your bowel is carefully examined.
During the colonoscopy, if the doctor sees something that may be abnormal, small amounts of tissue can be removed for analysis (called a biopsy), and abnormal growths, or polyps, can be identified and removed. In many cases, colonoscopy allows accurate diagnosis and treatment without the need for a major operation.
What Do I Need to Do Before a Colonoscopy?
Before a colonoscopy, let your doctor know about any special medical conditions you have, including the following:
- Pregnancy
- Lung conditions
- Heart conditions
- Allergies to any medications
If you have diabetes or take medications that may affect blood clotting; adjustments to these medications may be required before the colonoscopy.
Never stop taking any medication without first consulting your doctor.
You may need to take antibiotics before the colonoscopy if you:
- Have an artificial heart valve
- Have ever been told you need to take antibiotics before a dental or surgical procedure
How Do I Prepare for a Colonoscopy?
There may be some diet or fluid restrictions before you have a colonoscopy, but this will vary according to your doctor’s instructions. You may be asked to limit or eliminate solid foods for a few days before the test. You may also be asked to take laxatives by mouth.
Make sure you arrange for a driver to bring you home after the colonoscopy. Because you receive sedating medication during the procedure, it is unsafe for you to drive or operate machinery for 8 hours after the procedure.
What Happens After a Colonoscopy?
After your colonoscopy:
- You will stay in a recovery room for about 30 minutes for observation
- You may feel some cramping or a sensation of having gas, but this usually passes quickly
- You can resume your normal diet
Read your discharge instructions carefully. Certain medications, such as blood-thinning agents, may need to be avoided temporarily if biopsies were taken or polyps were removed.
Bleeding and puncture of the colon are rare but possible complications of colonoscopy. Call your doctor right away if you have any of the following:
- Excessive or prolonged rectal bleeding
- Severe abdominal pain, fever, or chills
