Overview Of Hysteroscopy
If you’re having heavy menstrual periods and severe cramping, or your doctor needs to know more about your reproductive health, they may recommend you have a hysteroscopy. The procedure can give them an up-close look at your cervix and uterus and help them learn what’s causing problems.
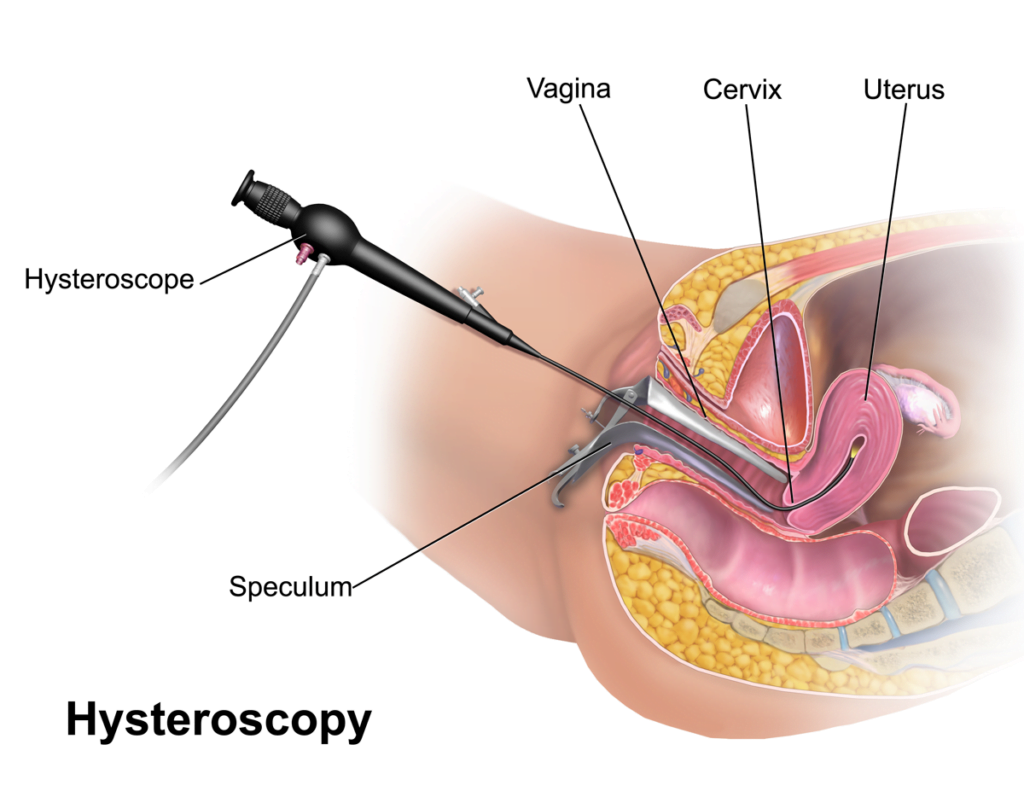
Hysteroscopy is the exam of the inside of the cervix and uterus using a thin, lighted, flexible tube called a hysteroscope. Your healthcare provider inserts the device through the vagina.
Your provider may use hysteroscopy to:
- Take a tissue sample (biopsy)
- Remove polyps or fibroid tumors
- Prevent bleeding by destroying tissue using electric current, freezing, heat, or chemicals
Your provider may do hysteroscopy in his or her office or in an outpatient center. You may have local or no anesthesia. Procedures that are more complex may be done in the operating room under local, regional, or general anesthesia.
Why might I need a hysteroscopy?
You may need a hysteroscopy for:
- Abnormal Pap test results
- Abnormal uterine bleeding
- Bleeding after menopause
- Diagnose the cause of infertility or repeated miscarriages
- Examine and remove uterine scarring, polyps, or fibroids
- Find and remove displaced IUDs (intrauterine devices)
- Place small birth control inserts into the fallopian tubes
- Removal of a small tissue sample (biopsy)
- Removal of endometrial lining
You can’t have a hysteroscopy if you are pregnant.
Your healthcare provider may have other reasons to do a hysteroscopy.
What are the risks for a hysteroscopy?
Some possible complications of hysteroscopy may include:
- Infection
- Bleeding
- Pelvic inflammatory disease
- Tearing of the uterus (rare) or damage to the cervix
- Complications from fluid or gas used to expand the uterus
You may have slight vaginal bleeding and cramps for a day or two after the procedure.
There may be other risks based on your condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
Certain things may interfere with a hysteroscopy. These include:
- Pelvic inflammatory disease
- Vaginal discharge
- Inflamed cervix
- Bloated bladder
How do I get ready for a hysteroscopy?
- Your healthcare provider will explain the procedure and you can ask questions.
- You may be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- Your provider may do a physical exam to be sure you are in good health. You may have blood tests or other diagnostic tests.
- You may be asked to fast before the procedure if you are to get local or general anesthesia. You may have local or regional anesthesia or no anesthesia. This depends on what other procedures your provider will do at the same time.
- If you are pregnant or think you could be, tell your healthcare provider.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, iodine, latex, tape, or anesthesia.
- Tell your healthcare provider of all medicines (prescription and over-the-counter) and herbal supplements that you are taking.
- Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any blood-thinning medicines (anticoagulants), aspirin, or other medicines that affect blood clotting. You may be told to stop these medicines before the procedure.
- You may get a sedative before the procedure to help you relax. If so, you will need someone to drive you home.
- You will be scheduled to have the procedure after your period and before ovulation. This lets your provider get the best view of the uterus. It also avoids harm to a new pregnancy.
- Dress in clothes that give access to the area or that are easily removed.
- Follow any other instructions your provider gives you to get ready.
What happens during a hysteroscopy?
Your provider may do a hysteroscopy an outpatient basis or during a hospital stay. Procedures may vary based on your condition and your healthcare provider’s practices.
Generally, a hysteroscopy follows this process:
- You will remove your clothing and put on a hospital gown.
- You will empty your bladder before the procedure.
- An intravenous (IV) line may be put in your arm or hand.
- You will be positioned on an operating table, lying on your back with your feet in stirrups.
- The vaginal area will be cleaned with an antiseptic solution.
- Your provider may dilate your cervix before inserting the hysteroscope.
- Your provider will insert the hysteroscope into the vagina, through the cervix, and into the uterus.
- Your provider will inject a liquid or gas through the hysteroscope to expand the uterus for a better view.
- Your provider will examine the wall of the uterus for problems. He or she may take photographs or videos and take tissue samples (biopsies).
- If you need a procedure, such as fibroid removal, your provider will insert tools through the hysteroscope.
- For more complex procedures, your provider may insert another type of scope through the belly (laparoscope) to view the outside of the uterus at the same time.
- When the procedure is done, your provider will remove the hysteroscope.
What happens after a hysteroscopy?
Your recovery will vary based on the type of anesthesia you have. If your provider used general anesthesia or a sedative, he or she will track your blood pressure, pulse, and breathing until they are stable and you are alert. When stable, you will be discharged to your home. Hysteroscopy is most often done on an outpatient basis.
Otherwise, you won’t need any special care after a hysteroscopy.
You may have cramping and vaginal bleeding for a day or two after the procedure. Report fever, severe abdominal pain, or heavy vaginal bleeding or discharge.
You may have gas in the digestive tract and pains from the gas given during the procedure. This can last for about 24 hours. You may also feel pain in your upper belly and shoulder.
Take a pain reliever for soreness as advised by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
Don’t douche or have sex for 2 weeks after the procedure, or as advised by your healthcare provider.
You can go back to normal activity and diet unless your healthcare provider tells you otherwise.
Your healthcare provider may give you other instructions based on your situation.
